Chinese Journal of Tissue Engineering Research ›› 2013, Vol. 17 ›› Issue (16): 3033-3040.doi: 10.3969/j.issn.2095-4344.2013.16.026
Long-term comparison of three bone graft materials in lumbar interbody fusion for lumbar spondylolisthesis
Yuan Zhen-chao, Chen Yuan-ming, Chen Feng, Liu Wan-xiang
- Department of Orthopedics, Ruikang Hospital, Guangxi University of Chinese Medicine, Nanning 530011, Guangxi Zhuang Autonomous Region, China
-
Received:2012-10-24Revised:2013-02-04Online:2013-04-16Published:2013-04-16 -
About author:Yuan Zhen-chao, Attending physician, Department of Orthopedics, Ruikang Hospital, Guangxi University of Chinese Medicine, Nanning 530011, Guangxi Zhuang Autonomous Region, China yzccwhyzw@163.com
CLC Number:
Cite this article
Yuan Zhen-chao, Chen Yuan-ming, Chen Feng, Liu Wan-xiang. Long-term comparison of three bone graft materials in lumbar interbody fusion for lumbar spondylolisthesis[J]. Chinese Journal of Tissue Engineering Research, 2013, 17(16): 3033-3040.
share this article
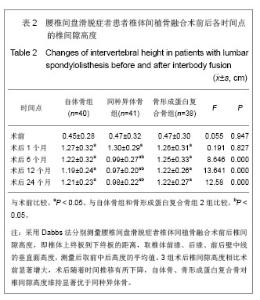
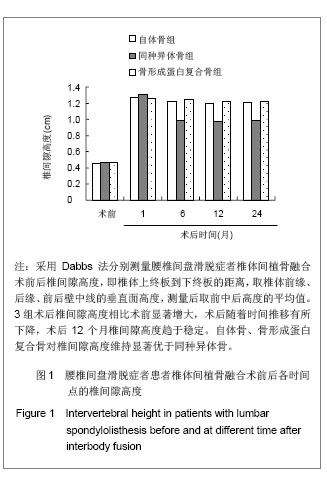
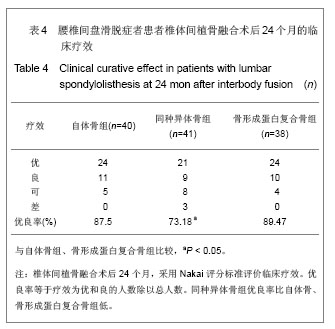
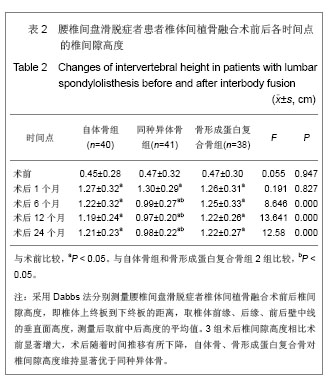
2.3 椎间隙高度的变化及比较 见表2和图1。术前自体骨组、同种异体骨组、骨形成蛋白复合骨组的椎间隙高度比较差异无显著性意义(P > 0.05),3组术后椎间隙高度相比术前显著增大,差异有显著性意义(P < 0.05)。术后椎间隙高度随着时间推移有所下降,术后12个月椎间隙高度趋于稳定。自体骨组、骨形成蛋白复合骨组术后各个观察时间点的椎间隙高度比较差异无显著性意义(P > 0.05)。术前与术后1个月,同种异体骨组椎间隙高度与自体骨组、骨形成蛋白复合骨组差异无显著性意义(P > 0.05);术后6,12,24个月,同种异体骨组椎间隙高度比自体骨组、骨形成蛋白复合骨组低,差异有显著性意义(P < 0.05)。说明自体骨、骨形成蛋白复合骨对椎间隙高度维持显著优于同种异体骨,自体骨、骨形成蛋白复合骨2种植骨材料对椎间隙高度维持无明显差异。"
| [1]Marchi L, Oliveira L, Coutinho E, et al. Results and complications after 2-level axial lumbar interbody fusion with a minimum 2-year follow-up. J Neurosurg Spine. 2012;17(3): 187-192.[2]Smoljanovic T, Dokuzovic S, Bojanic I. Osteoinductive bone graft substitutes for lumbar fusion. J Neurosurg Spine. 2010; 13(3):407-409. [3]Agarwal R, Williams K, Umscheid CA, et al. Osteoinductive bone graft substitutes for lumbar fusion: a systematic review. J Neurosurg Spine. 2009;11(6):729-740. [4]König MA, Boszczyk BM. Limited access surgery for 360 degrees in-situ fusion in a dysraphic patient with high-grade spondylolisthesis. Eur Spine J. 2012;21(3):390-395.[5]Chrastil J, Patel AA. Complications associated with posterior and transforaminal lumbar interbody fusion.J Am Acad Orthop Surg. 2012;20(5):283-291.[6]Schmid R, Lindtner RA, Lill M, et al. Combined posteroanterior fusion versus transforaminal lumbar interbody fusion (TLIF) in thoracolumbar burst fractures. Injury. 2012;43(4):475-479. [7]Wei C, Yang HL, Wang GL, et al. Zhongguo Zuzhi Gongcheng Yanjiu yu Linchuang Kangfu. 2009;13(52):10274-10278.魏超,杨惠林,王根林,等.椎间融合与环周融合结合椎弓根钉内固定置入治疗成人腰椎滑脱:效果优于后外侧融合吗[J]?中国组织工程研究与临床康复,2009,13 (52):10274-10278.[8]Jensen SS, Terheyden H. Bone augmentation procedures in localized defects in the alveolar ridge: clinical results with different bone grafts and bone-substitute materials. Int J Oral Maxillofac Implants. 2009;24 Suppl:218-236.[9]Khojasteh A, Behnia H, Shayesteh YS, et al. Localized bone augmentation with cortical bone blocks tented over different particulate bone substitutes: a retrospective study. Int J Oral Maxillofac Implants. 2012;27(6):1481-1493.[10]Bose S, Roy M, Bandyopadhyay A. Recent advances in bone tissue engineering scaffolds. Trends Biotechnol. 2012;30(10): 546-554. [11]Zimmermann G, Moghaddam A. Allograft bone matrix versus synthetic bone graft substitutes. Injury. 2011;42 Suppl 2:S16-21. [12]Sun Y, Meng QF, Gao ZH, et al. Yingxiang Zhenduan yu Jieru Fangshexue. 2007;16(3):135-137.孙洋,孟悛非,高振华,等.椎间盘和椎间隙的影像学对比观察[J].影像诊断与介入放射学,2007,16(3):135-137.[13]Suk SI, Lee CK, Kim WJ, et al. Adding posterior lumbar interbody fusion to pedicle screw fixation and posterolateral fusion after decompression in spondylolytic spondylolisthesis. Spine. 1997;22(2):210-219;discussion 219-220.[14]Zhang JG, Ding WY, Shen YY. Jizhu Waike Zazhi. 2011;9(4): 232-235.张剑刚,丁文元,申摇勇.经椎间孔椎体间融合术治疗复发性腰椎椎间盘突出症的疗效分析[J].脊柱外科杂志,2011,9(4):232-235. [15]Wang LL, Jin GL, Ren LL, et al. Zhongguo Zuzhi Gongcheng Yanjiu yu Linchuang Kangfu. 2011;15(16):2885-2888.王磊磊,金格勒,任龙龙,等.不同植骨材料在腰椎融合过程中的应用及转化生长因子β的表达[J].中国组织工程研究与临床康复, 2011,15(16):2885-2888.[16]Yang Y, Jin GL,Tang ZZ, et al. Zhonghua Shiyan Waike Zazhi. 2010;27(2):245-247.杨毅,金格勒,唐周舟,等.复合骨在兔腰椎融合过程中相关基因表达调控的影响[J].中华实验外科杂志,2010,27(2):245-247.[17]Guo CT, Zhou Q, Dai F, et al. Disan Junyi Daxue Xuebao. 2010;32(17):1875-1879.郭从涛,周强,代飞,等.异体腓骨环椎间融合器在腰椎融合术中的效果分析[J].第三军医大学学报,2010,32(17):1875-1879.[18]Zhang HB, Wang YS,JIA SM, et al. Zhongguo Jiaoxing Waike Zazhi. 2008;16(9):657-659.张海波,王义生,贾思明,等.后路环状融合术在腰椎滑脱症外科手术中的应用[J].中国矫形外科杂志,2008,16(9):657-659.[19]Yin P, Liu XZ, Wu YP, et al. Zhongguo Xiufu Chongjian Waike Zazhi. 2012;26(7):778-782.殷鹏,刘秀珍,吴延平,等.不同植骨材料在退变性腰椎病脊柱融合术中的应用与疗效比较[J].中国修复重建外科杂志, 2012, 26(7): 778-782.[20]Ito Z, Matsuyama Y, Sakai Y, et al. Bone union rate with autologous iliac bone versus local bone graft in posterior lumbar interbody fusion. Spine (Phila Pa 1976). 2010;35(21): E1101-E1105. [21]Liao SS, Guan K, Cui FZ, et al. Lumbar spinal fusion with a mineralized collagen matrix and rhBMP-2 in a rabbit model. Spine (Phila Pa 1976). 2003;28(17):1954-1960.[22]Luo J, Sun MH, Kang Q, et al. Gene therapy for bone regeneration. Curr Gene Ther. 2005;5(2):167-179.[23]Kai T, Shao-qing G, Geng-ting D. In vivo evaluation of bone marrow stromal-derived osteoblasts-porous calcium phosphate ceramic composites as bone graft substitute for lumbar intervertebral spinal fusion. Spine (Phila Pa 1976). 2003;28(15):1653-1658.[24]Ma X, Wu, XM, Hu YY, et al. Intervertebral Spinal Fusion Using a RP-based PLGA/TCP/bBMP Biomimetic Grafting Material. J Bioact Compat Pol. 2009;24(1):146-157.[25]Zou X, Zou L, Foldager C, et al. Different mechanisms of spinal fusion using equine bone protein extract, rhBMP-2 and autograft during the process of anterior lumbar interbody fusion. Biomaterials. 2009;30(6):991-1004.[26]Fei QM, Jiang XX, Chen TY, et al. Changes with age and the effect of recombinant human BMP-2 on proteoglycan and collagen gene expression in rabbit anulus fibrosus cells. Acta Biochim Biophys Sin (Shanghai). 2006;38(11):773-779.[27]Kong MH, Do DH, Miyazaki M, et al. Rabbit Model for in vivo Study of Intervertebral Disc Degeneration and Regeneration. J Korean Neurosurg Soc. 2008;44(5):327-333.[28]Gu Y, Chen L, Yang HL, et al. Evaluation of an injectable silk fibroin enhanced calcium phosphate cement loaded with human recombinant bone morphogenetic protein-2 in ovine lumbar interbody fusion. J Biomed Mater Res A. 2011;97(2): 177-185.[29]Ma X, Hu YY, Lv R, et al. Multilevel Posterior Lumbar Interlaminar Fusion in Rabbits Using Bovine Bone Protein Extract Delivered by a RP-synthesized 3D Biopolymer Construct. J Bioact Compat Pol. 2010;25(5):513-526.[30]Wang XY, Guo X, Qu SX, et al. Temporal and spatial CGRP innervation in recombinant human bone morphogenetic protein induced spinal fusion in rabbits. Spine (Phila Pa 1976). 2009;34(22):2363-2368. |
| [1] | Yao Rubin, Wang Shiyong, Yang Kaishun. Minimally invasive transforaminal lumbar interbody fusion for treatment of single-segment lumbar spinal stenosis improves lumbar-pelvic balance [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1387-1392. |
| [2] | Wang Haiying, Lü Bing, Li Hui, Wang Shunyi. Posterior lumbar interbody fusion for degenerative lumbar spondylolisthesis: prediction of functional prognosis of patients based on spinopelvic parameters [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1393-1397. |
| [3] | Liang Yan, Zhao Yongfei, Xu Shuai, Zhu Zhenqi, Wang Kaifeng, Liu Haiying, Mao Keya. Imaging evaluation of short-segment fixation and fusion for degenerative lumbar scoliosis assisted by highly selective nerve root block [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1423-1427. |
| [4] | Liu Zhengpeng, Wang Yahui, Zhang Yilong, Ming Ying, Sun Zhijie, Sun He. Application of 3D printed interbody fusion cage for cervical spondylosis of spinal cord type: half-year follow-up of recovery of cervical curvature and intervertebral height [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 849-853. |
| [5] | Liu Lihua, Sun Wei, Wang Yunting, Gao Fuqiang, Cheng Liming, Li Zirong, Wang Jiangning. Type L1 steroid-induced osteonecrosis of the femoral head through femoral head and neck junction decompression by fenestration: a single-center prospective clinical study [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 906-911. |
| [6] | Hua Haotian, Zhao Wenyu, Zhang Lei, Bai Wenbo, Wang Xinwei. Meta-analysis of clinical efficacy and safety of antibiotic artificial bone in the treatment of chronic osteomyelitis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 970-976. |
| [7] | Fu Shuanhu, Qin Kai, Lu Dahan, Qin Haibiao, Gu Jin, Chen Yongxi, Qin Haoran, Wei Jiading, Wu Liang, Song Quansheng. Lumbar spinal tuberculosis implanted with artificial bone with streptomycin sulfate and percutaneous pedicle screw under transforaminal endoscopy [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 493-498. |
| [8] | Li Li, Ma Li. Immobilization of lactase on magnetic chitosan microspheres and its effect on enzymatic properties [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 576-581. |
| [9] | Liang Yan, Zhao Yongfei, Zhu Zhenqi, Liu Haiying, Mao Keya. Minimally invasive transforaminal lumbar interbody fusion in the treatment of sciatic scoliosis caused by lumbar disc herniation: a 2-year follow-up of coronal and sagittal balance [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 409-413. |
| [10] | Xing Hao, Zhang Yonghong, Wang Dong. Advantages and disadvantages of repairing large-segment bone defect [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 426-430. |
| [11] | Zhou Anqi, Tang Yufei, Wu Bingfeng, Xiang Lin. Designing of periosteum tissue engineering: combination of generality and individuality [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3551-3557. |
| [12] | Lang Limin, He Sheng, Jiang Zengyu, Hu Yiyi, Zhang Zhixing, Liang Minqian. Application progress of conductive composite materials in the field of tissue engineering treatment of myocardial infarction [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3584-3590. |
| [13] | Wang Renxian, Cao Jingjing, Wang Honggang, Wan Ben, Liu Weifeng. Effects of dispersants on aggregation, intracellular distribution and cell proliferation of nano-hydroxyapatite [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(16): 2500-2505. |
| [14] | Xie Jian, Su Jiansheng. Advantages and characteristics of electrospun aligned nanofibers as scaffolds for tissue engineering [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(16): 2575-2581. |
| [15] | Ji Qi, Yu Zhengwen, Zhang Jian. Problems and trends of technique and clinical application of metallic biomaterials prepared by three-dimensional printing technology [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(16): 2597-2604. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||